Vulvovaginal Atrophy
 Vulvovaginal atrophy (VVA) is a common condition associated with the decreased estrogenization of the vaginal tissues. It occurs most often after menopause, but it can also develop during breast-feeding or at any other time your body’s estrogen production declines.
Vulvovaginal atrophy (VVA) is a common condition associated with the decreased estrogenization of the vaginal tissues. It occurs most often after menopause, but it can also develop during breast-feeding or at any other time your body’s estrogen production declines.
The inevitable estrogen deficiency that accompanies reproductive aging and menopause results in universal changes in the vaginal ecosystem associated with a variety of vulvovaginal and urogenital complaints. At some point in their lives, the majority of women will experience these symptoms, collectively termed the genitourinary syndrome of menopause (GSM), a term which has recently replaced vulvovaginal atrophy (VVA) in the accepted nomenclature. VVA or GSM symptoms usually develop gradually and become most bothersome as women transition to the mid-to-late 50’s. These symptoms typically follow the vasomotor symptoms of menopause, such as hot flashes and night sweats. Unlike VMS, which usually subside after several years, the symptoms of GSM (see below) persist and increase in both frequency and intensity as women age.
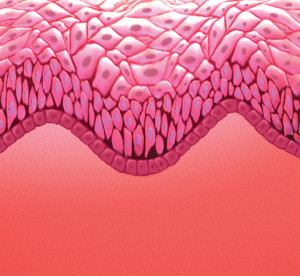
With estrogen deficiency, the epithelium (aka the surface cells) of the vagina and vulva thins and loses its rugal folds. Those folds are really important. Think of the difference between a pair of pants with elastic, or a skirt with pleats vs one without. Imagine how you would feel trying to put them on if you’ve gained 20 pounds. Which pants would you like to squeeze into? With menopause and increasing VVA or GSM, the elasticity provided by those rugal folds diminishes, and susceptibility to injury, even with minor trauma, can ensue. Estrogen deficiency also leads to diminished vaginal glycogen and decreased acidity of the vaginal secretions (increased pH), thereby reducing the vagina’s natural defense against local pathogens (i.e. yeast and coliforms [the most common bacteria of fecal material]). The close proximity of the lower urinary tract to fecal contamination is associated with an increased risk for acute and recurrent urethritis and cystitis (bladder infections).
When a woman doesn’t have intercourse or other vaginal sexual activity on a regular basis following menopause, her vagina may also become shorter and narrower. Continuing to have regular vaginal sexual activity through menopause helps keep the vaginal tissues thick and moist and maintains the vagina’s length and width. This can help keep sexual activity pleasurable. This has euphemistically been referred to as “use it or lose it”.
If you do experience vulvovaginal symptoms (dryness, irritation, burning, itchiness, pain) do not automatically assume that reduced estrogen levels are the reason for these symptoms. Because vaginal discomfort can arise from many different sources, persistent symptoms should be brought to the attention of your healthcare provider for evaluation.
Interested in women’s sexual health? Contact us for an appointment.
